Chapter 1
After your surgery, you are going to need to follow a gastric sleeve diet. Gastric sleeve surgery is the first big step in your weight loss journey and the diet will be the most crucial part of it. It is very important to stick to it. It will benefit your healing process and help you get the nutrients you need to become healthier.
In some cases, gastric sleeve patients may also need a pre-op diet. Or they might want to start early. So they need or require a more inclusive gastric sleeve diet plan for pre-op and post-op. We got you, let’s talk about it in detail.
Nutrition guide to the diet before gastric sleeve
Here you are preparing for the surgery. You may need the preoperative diet for gastric sleeve to shrink your liver and/or lower your BMI. This way the surgery can be easier and safer to perform.
You are not only preparing yourself for the surgery with a pre-op diet but you are also getting used to your new lifestyle and preparing for the post-op diet. This way, you can adapt to it way easier.
If you’re engaging in bad eating habits, you should discontinue them during your pre-op diet. These habits include consuming fast foods, bread products, sugary and carbonated beverages, alcohol, caffeinated beverages, and smoking.
You need a good pre op diet plan for two weeks. Your approximate calorie intake for this sleeve diet should be between 1200-1400. No higher, no lower.
You can find here our complete guide on pre op diet (Chapter 2).
Nutrition guide to the diet after gastric sleeve
You had the surgery and all is going well. Let’s see what the gastric sleeve diet has in store for you.
After the surgery, your stomach needs time to heal. And to achieve that, the stomach needs to rest. That is why the progression has been split into 5 stages. The patient will go from liquid to solid approximately in a month with this diet plan for gastric sleeve. It is absolutely important to stick to this diet. Eating food that you are not allowed to may increase the risk of complications.
You should keep yourself hydrated during the whole process. 1,5-2 liters of water a day is the ideal amount for you to drink. That does not include tea and broth. You should consume plain water.
You will also be getting nutritional supplements for 1-2 months and multivitamin supplements for 6 months after your surgery. These will be essential to maintain long-term weight loss.
You will have to wait 30 mins to drink liquids between meals: 30 mins before the meal and 30 mins after the meal. You can not drink and eat at the same time or immediately after.
You can find here our complete guide on post-op diet (Chapter 3).
The post-op diet stages
Here are the five stages of gastric sleeve post op diet that will last for a month. Each stage has its own restrictions and instructions.
Stage 1:
This is the all-clear liquid stage. It lasts 10 days. With this stage, you will also be getting your blood thinner injection/medicine.
You can consume clear liquids that have no food particles inside them. Such as broth, tea, and protein water. You can have fresh fruit juices without added sugar.
Stage 2:
10 days have passed. Now it’s time for soups and lactose-free/non-fat milk! You will be doing a semi–liquid semi–puree diet. Restrictions from the 1st stage remain the same in this stage. This stage is a transition stage and it will last 3 days.
Stage 3:
Straight out of stage 2, you are ready for a puree diet. Rules and restrictions are of course the same. In this stage, make sure that you blend your food well. You can now have more types of dairy products. Solid stuff can disturb your stomach and can even lead to leakage. This stage will last 1 week.
Stage 4:
Look at you go. Already at stage 4. This stage is the preparation period for solid food. It is not long before you can eat solid food.
You can add some flavor to some of your food now! You can add some spices to your protein shake! Cocoa powder, cinnamon powder, and sugar-free vanilla powder are some of the great options.
In this dietary stage, you will be able to eat lean meats and low-fat fish However, these meats need to be blended or crushed/smushed well as you are not in the solid food stage yet. Especially red meat. You still need to eat them as ground beef. You will need to chew your food well and start the digestion process in your mouth so that the stomach can have an easier time digesting.
This stage will last 1-2 weeks, depending on your food tolerance.
Stage 5:
Finally, a solid diet! Now, you can have meat without shredding or blending them. However, red meat is still a tough one to digest. So, you still need to have it as ground beef. You still cannot consume certain spices and raw vegetables and fruits. You will be allowed to have them after your 1-month checkpoint, or when your dietitian says it is okay for you to do so.
This stage will last until 3 months after your discharge.
Before we dive in here are some tips to keep in mind
Well, now you have some insight about what to eat and for how long. Let’s talk about how you cook and have much you eat can affect your gastric sleeve diet. Not everyone can or will eat the same things.
Some may like cottage cheese, some may be lactose intolerant. Meanwhile, cheddar cheese is considered to be lactose-free, but it has too many calories. Did you know that there are 400 calories in 100g of cheddar cheese? It’s crazy!
So it is important to arrange a diet program personally prepared for you regarding your digestive system and calorie intake. Let’s dig deeper!
Cooking style matters
How you cook your meals can change the course of your diet. For instance, you shouldn’t be using animal-based oil in your meals. You can use 3 spoons of extra virgin olive oil with 1 portion of your food or you can simply eat olives that are not too salty. Olives or olive oil can help with constipation, which you may experience after gastric sleeve surgery.
Of course, there are also cultural foods and spices. For instance, Indian food is known to be very spicy. After a gastric sleeve surgery, most of the spices in an Indian dish are not allowed for a recovering patient. Before going for your cultural food, no matter how healthy they are, you should consult your dietitian. They will be in constant touch with you during your recovery.
Of course, you might like to eat something crispy, and crisps are usually achieved by frying the food. Deep frying is a big no-no. If you would like to eat something crispy, during and after your 5th stage, you can bake them or you can use an air fryer to fry them. This way, you will use less oil in your meals.
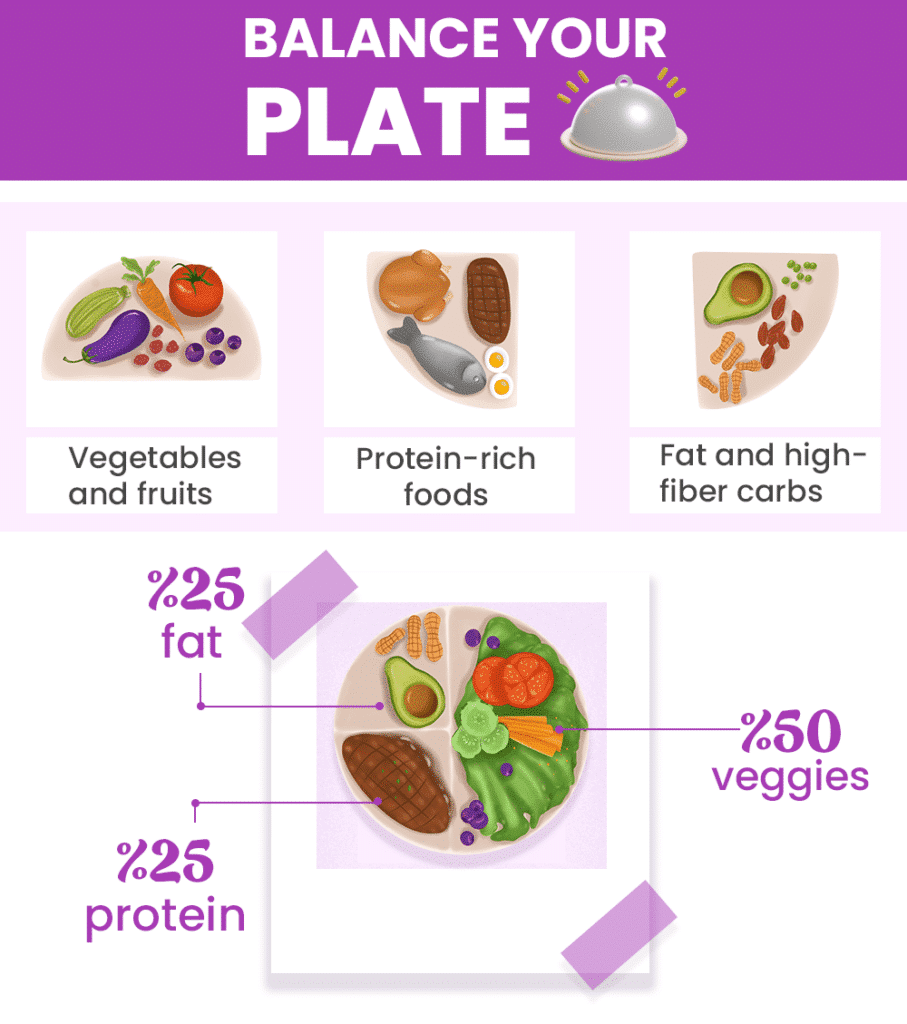
You should know how to balance your plate
There are certain amounts of each food group you need to consume. If you consume less, you will be malnourished and that will affect your recovery negatively. If you consume more, it will also affect your recovery negatively and also can cause your stomach to stretch.
Here’s an example of what your plate should look like:
- Get a dessert plate (approx. 9-10 inches)
- Fill half of it with your low-starch vegetables
- Fill a quarter of the plate with your lean meats (approximately 60 grams of protein)
- Lastly, fill the rest of the plate with healthy carbohydrates, such as fiber-rich peas.
You will get the hang of portion control in time. Do not worry. You’ll be a pro even when eating out after a sleeve.
How long does it take to digest your meal?
“Why are we eating so many veggies and proteins?” “Why can’t I eat rice?” It can be healthy if eaten moderately…” So many questions, so many answers. Let’s break it down for you:
- Complex carbs, such as fiber-rich veggies like peas, take 1 hour to digest
- Protein takes approximately 3-4 hours to digest
- White rice, white bread, etc. takes 30 minutes to digest
Long story short, if you eat white carbs that get digested in 30 minutes, you will feel hungry again in a short period of time. They also raise your sugar levels more than they should and high sugar levels for a long period of time can lead to insulin tolerance. Consequently, that may lead to diabetes. We’re trying to overcome it or prevent that from happening.
References:
(1.) Bray GA, Frühbeck G, Ryan DH, Wilding JPH. Management of obesity. The Lancet. 2016;387(10031):1947-1956. doi:10.1016/s0140-6736(16)00271-3 Link
(2.) Tabesh MR, Maleklou F, Ejtehadi F, Alizadeh Z. Nutrition, Physical Activity, and Prescription of Supplements in Pre- and Post-bariatric Surgery Patients: a Practical Guideline. Obesity Surgery. 2019;29(10):3385-3400. doi:10.1007/s11695-019-04112-y Link
(3.) Garvey WT, Mechanick JI, Brett EM, et al. AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS AND AMERICAN COLLEGE OF ENDOCRINOLOGY COMPREHENSIVE CLINICAL PRACTICE GUIDELINES FOR MEDICAL CARE OF PATIENTS WITH OBESITY. Endocrine Practice. 2016;22(Supplement 3):1-203. doi:10.4158/ep161365.gl Link