- Introduction: Gastric sleeve
- Chapter 1: What is gastric sleeve?
- Chapter 2: Gastric Sleeve requirements
- Chapter 3: Gastric Sleeve procedure (you’re here)
- Chapter 4: Gastric Sleeve recovery
- Chapter 5: Gastric Sleeve complications
- Chapter 6: Gastric Sleeve regrets
- Chapter 7: Gastric Sleeve cost
- Chapter 8: Gastric Sleeve Turkey
- Chapter 9: Gastric Sleeve Revision
Chapter 3
Gastric sleeve procedure is a highly demanded and effective weight loss surgery. Approximately, 150 thousand people per year get gastric sleeve surgery. It is a minimally-invasive surgery that has turned thousands of lives around. You probably know by now what’s a gastric sleeve and what can it do for you. But how is it performed?
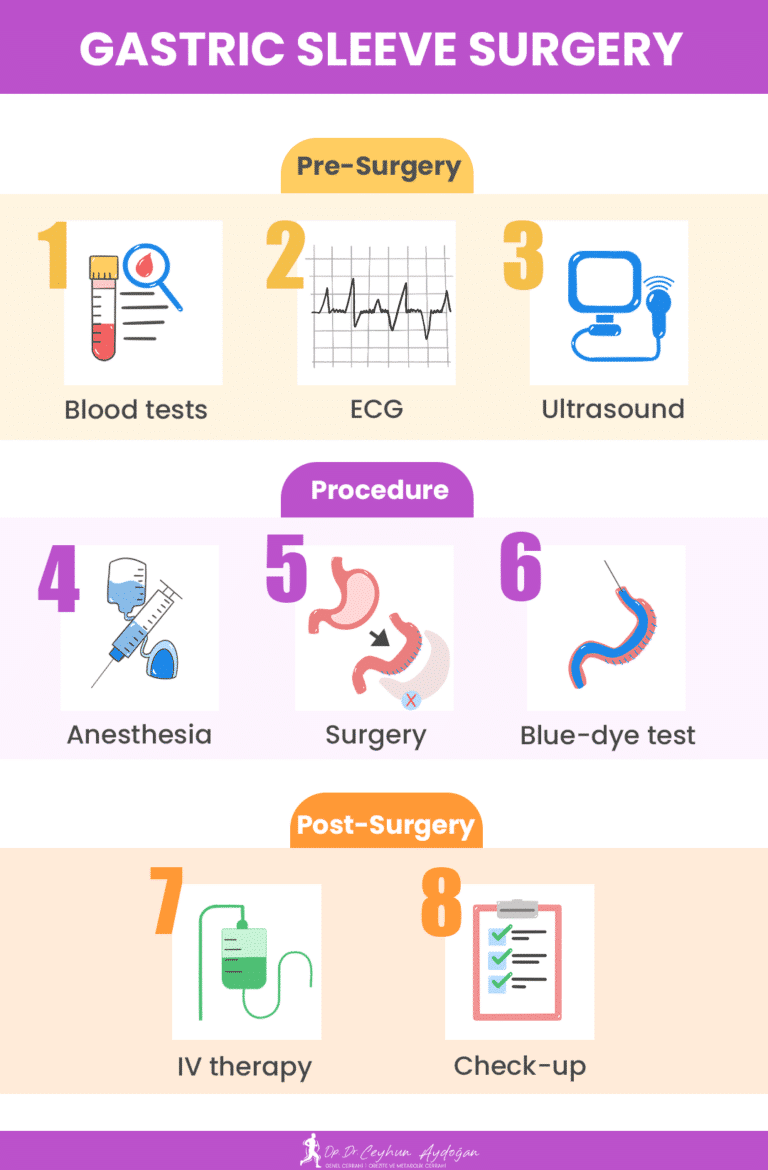
In this chapter, we will talk about how to prepare for the surgery, how the surgery is performed step-by-step along with other types of gastric sleeve operations, and how post-operative care is performed.
Without any more suspense, let’s dive right in.
Before the surgery: what happens?
The night before the gastric sleeve procedure is the night you should do your last preparations. You will be in the hospital for 2-3 nights. So you should pack accordingly.
You should stop eating and drinking usually 12 hours before your surgery. This is to ensure the stomach is empty. It is because anesthesia stops the body’s reflexes during the surgery.
Some tests will be performed on you on the day of surgery. Vascular access will be opened on the top of your hand for serums. You can ask to get them on your arm if that is more comfortable for you.
The tests that will be performed on you are blood tests, electrocardiogram (ECG), and ultrasound. With these tests, the surgeon and the anesthesiologist will determine the course they are going the take during the procedure. After they are all cleared, you will be sent back to your hospital room to change into your surgery gown and remove all your jewelry.
Nurses will take you to a waiting area near the operating rooms where you will be put to sleep.
Gastric sleeve procedure step by step
During the gastric sleeve procedure, your surgeon will make five incisions on your abdomen to let the instruments in and cut and staple your stomach, making it into a smaller sleeve shape. After that, the extra stomach tissue will be taken out. Finally, your surgeon will check everything and remove the tools, and you’ll be injected with local anesthetics for any pain.
Let’s start by explaining the steps in order.
Step 1: preparing the patient
You will be positioned on the operating table facing upward (supine) in the T position. And then the table will be tilted forward. This position is called Reverse Trendelenberg. The surgical team will cover you with sheets in a way that only your abdomen and your face are exposed. Afterward, you will be intubated to aid your breathing.
Before applying anesthesia, your stomach will be checked via upper endoscopy. Carbon dioxide (CO2) will be pumped into your stomach to inflate it for better vision and movement for the endoscope. An instrument called French bougie will later be inserted in your stomach through your mouth to guide the endoscopic linear stapler around the sleeve that is about to be your stomach. After it has been placed, excess air will be sucked out and you will be given general anesthetics.
3–5 incisions will be made on your abdomen. Through one of the incisions, your abdomen will be inflated with carbon dioxide. This will provide better vision and movement for the surgeon to perform the surgery.
Step 2: the gastric sleeve procedure
Once the surgical instruments are in place, your surgery will begin. First, the surgeon will separate the stomach from adhesions and fatty tissue. Then, your stomach will be reduced in size by cutting and stapling with an endoscopic linear stapler. The staples for this surgery will remain on your stomach permanently.
After the gastrectomy is complete, if needed, your surgeon will suture the staple line on the stomach that is now a sleeve. The excess stomach tissue will later be removed through one of the incisions. Finally, the surgeon will do the last observations.
Step 3: blue dye test
Before stitching the incisions made on your abdomen, your surgeon will give you some methylene blue (blue water). After that, the surgeon will check if there are any staple line leaks on the staple line either endoscopically or laparoscopically. This is to avoid leaking as a gastric sleeve complication. If the leakage is not fixed in time, the surgeon may need to consider a gastric sleeve revision surgery to fix the problem.
The trochars and other tools will be removed and your surgeon will inject local anesthetics into the surgical site. Through one of the incisions made on your abdomen, the pumped carbon dioxide will be extracted. When it is all done, all of the incisions will be stitched and bandaged; and 1 or 2 drains will be inserted through certain incisions.
Proceedings of other types of gastric sleeve
Other types of bariatric sleeve surgeries may proceed a bit differently. To elaborate:
- Laparoscopic Gastric Sleeve: Also known as the traditional gastric sleeve. 80% of the stomach is removed via a laparoscope and endoscopic linear stapler.
- Mini Gastric Sleeve: A mini gastric sleeve is a laparoscopic gastric sleeve on a smaller scale. Around 40%-50% of your stomach will be removed.
- Robotic Gastric Sleeve: This robotic surgery is basically a laparoscopic gastric sleeve performed via a robotic platform controlled by a surgeon. Although not preferred, it can provide better dexterity and vision for the surgeon. 60%-80% of the stomach can be removed with this procedure.
- Endoscopic Gastric Sleeve: This procedure is done via an endoscope. The stomach is narrowed by about 70% in size by sutures instead of being cut and removed. This procedure is less invasive than other methods.
Endoscopic surgery: It is a technique that utilizes an endoscope, which is a thin and flexible tube with a camera and light attached to it. This instrument is inserted through the throat and into the stomach, and allows the surgeon to view the internal organs without making any incisions.
Right after surgery
After you are done with the procedure, on your way to your room, the bariatric team will start waking you up. You may be conscious when you enter your room. This is where the gastric sleeve recovery time starts.
IV therapies
During your hospital stay, you will not be able to use medications or take nourishment orally. Instead, you will be given IV drips for nutrition, rehydration, pain relief, stomach protection (stomach acid balancer), prevention of infection, and clotting.
You can also get IV therapies after being discharged if you are experiencing certain side effects. Such as dumping syndrome, indigestion, or nausea and vomiting. These side effects can cause another side effect; nutrient and vitamin deficiencies. These can be managed via IV therapy.
Post-op tests
While you are in the hospital, your vitals and the drain(s) inserted into one of the incisions on your abdominal wall will be checked regularly for your postoperative care. After you have been mobilized, you will be checked if you are experiencing any problems, such as high blood pressure.
Right before being discharged, you will be given methylene blue again. After that, you will be sent to get an X-Ray to see if there are any leaks. If there are, it will be taken care of. If not, you will be given instructions about your recovery and will be sent home to continue your journey.
On your 6th, 9th, and 12th–month checkpoints, your surgeon may ask you for blood tests to observe your blood count and to see if your body is lacking certain nutrients. If so, your diet will be rearranged accordingly.
Chung AY, Thompson R, Overby DW, Duke MC, Farrell TM. Sleeve Gastrectomy: Surgical Tips. Journal of Laparoendoscopic & Advanced Surgical Techniques. 2018;28(8):930-937. doi:10.1089/lap.2018.0392
Seeras K, Sankararaman S, Lopez PP. Sleeve Gastrectomy. PubMed. Published 2022. Accessed March 3, 2023. https://pubmed.ncbi.nlm.nih.gov/30085577/
Abu-Jaish W, Rosenthal RJ. Sleeve gastrectomy: a new surgical approach for morbid obesity. Expert Review of Gastroenterology & Hepatology. 2010;4(1):101-119. doi:https://doi.org/10.1586/egh.09.68